Wound Care
What is a surgical wound?
Surgical wounds are incisions through the skin during surgery. Wound edges are kept together with wound closure steristrips, sutures or staples. Sometime small wounds , after a shave biopsy and curettage, are not closed directly and left alone to be healed up spontaneously. This is called secondary intention healing.
Caring for your wound after your skin procedure is important to help prevent infection and help heal your wound.
what are the common complications of skin surgery?
Skin cancer surgeries like any other operations have risks and can develop complications. Main complications of the skin cancer surgery are:
- swelling and bruising, especially for wounds around the eyes and nose.
- bleeding,
- infection,
- numbness,
- scar,
- skin tightening or stretching.
Pain. For reducing your pain, you could take Paracetamol ( panadol, panadeine) . Do not take aspirin as this may increase the risk of bleeding. If pain and redness don’t subside after two days or if the wound starts to drain, you may have an infection and you should contact your doctor soon.
Bleeding. The surgical area may ooze a little blood or clear liquid especially in the first few hours after surgery. Hot drinks or bending over at the waist can also initiate or worsen bleeding of face wounds. If bleeding occurs, firm pressure applied directly to the site for 10 minutes may be helpful. If dressing becomes soaked with bright red blood, remove the dressing, and apply gentle but firm direct pressure to the wound for 10 minutes using a piece of clean gauze. Avoid “peeking” during this period. Check wound again and repeat procedure one more time if there is still bleeding. If the bleeding stops, clean your surgery site, apply vaseline ointment and cover with clean dressing. If bleeding continues despite 30 minutes of pressure, please call us or after hours doctor.
Swelling. Swelling commonly occur after surgery. Swelling is more common for surgeries around the eyes or lips. Sleeping propped up on a few pillows or in a reclining chair may help decrease swelling after surgery of the head and face area. You can reduce swelling by applying ice packs on the area for 10 minutes, every hour for up to 24 hours after surgery.
Bruising: If your surgical area is near the eye or forehead, you may experience a black eye and swelling around the eye within 48 hours of the surgery. This is not a sign of active bleeding and will improve after a few days.
Scar. scar is always larger than the size of the skin cancer. Scar of flaps and grafts have geometric shapes like W, Z or T. Scarring from the surgery usually improve with time. It could take several months for the scar of flaps and graft to look better. Sometimes due to the extent of skin cancer you need to have a larger reconstruction which may end up in a more obvious scar.
Nerve damage can occur but is usually temporary. However it can be permanent if the cancer is extensive and the nerve is involved.

What should I do after the surgery?
It is important to look after your wound skin surgery to help prevent infection and promote healing. It may be advisable to avoid heavy lifting and exercise, especially the first 24-48 hours after surgery. You should keep the area dry for 24 hours. Swimming pools, oceans, and Jacuzzis are usually not permitted while the stitches are in. Sutures will be removed in 5 – 14 days after the surgery. Doctor will inform you of the time to remove the sutures.
- Avoid strenuous physical activities such as swimming, running for at least 2 weeks after surgery
- Reduce or stop smoking as smoking causes poor wound healing
- Sleep with your head elevated to reduce swelling if surgical site is on the face
- If the surgery was on your face, avoid hot drinks for the 1st day and do not bend over for the first few days but rather squat if you need to reach down.
- Try to avoid applying makeup or powder directly on a fresh wound unless the surface is fully healed.
- You may notice discolouration of skin (pinkness/redness) at the site of surgery for up to a year after your surgery. Once the site has healed up, you should apply a broad-spectrum sunscreen with an SPF 30+ and moisturiser to protect it from scarring.

Wound care at home
Observe the following guidelines to help your surgical wounds and biopsies heal quickly, successfully and with less scarring:
- Leave the bandage on your wound for 24 hours and keep it clean and dry.
- You can apply an ice pack to the site for few minutes several times during the first 24 hours after your surgery . This will reduce bleeding, pain, and swelling after surgery.
- You can have a shower 24 hours after your surgery but do not soak your wound in a bath or allow the shower stream to directly wet your wound.
- Please do not immerse the wound under water (bath, hot tub, swimming pool, …) until one week after sutures are removed.
- If you have Steri-Strips over your wound, do not remove them. They will fall off on their own by slowly curling off in about 1 week. Trim the curled edges and within a few days, the entire strip should come off.
- Please keep movement of the surgical site to a minimum for the first three weeks after surgery. Wounds only have approximately 5% of their strength one week after surgery and so care must be taken not to stretch open the surgical site. Avoid stretching or overusing the surgical area for three weeks and then slowly start to increase activity to the affected area.

Wound care instructions
- Wash your hands with soap and warm water or use an alcohol-based hand sanitizer
- Gently wash the wound with soap and water to remove the crust. Do not scrub or soak the wound.
- Gently pat your wound dry with a clean gauze pad.
- Use cotton applicators to put petrolatum ointment/Vaseline ointment on your wound. Keep ointment on the wound at all times until the wound is healed. Crusting and scabbing will impede healing and may produce a more noticeable scar.
- Cover your wound with a dressing or a bandage cut to the size of your wound. Most wounds may be left uncovered after five to seven days. However, wounds that are on an area of the body that becomes easily irritated should be covered with a bandage during the daytime for additional 5-7 days.
- Wash your hands with warm water and soap or use an alcohol-based hand sanitizer.
- Follow these instructions every day till sutures are removed.If you have a skin graft, keep the dressing dry and intact for 5-10 days until you are seen in clinic again. Our nursing staff will remove the dressing at that time.
Should I be worried about
Wound healing is usually straighforward and ununcomplicated if you carefully follow the wound care instructions by your doctor.
About 1% of wounds could be complicated such as wound infection, wound breakdown, bleeding etc,
Call the clinic if you notice:
- A temperature of 38 ° C or higher
- Chills
- Any of the following symptoms at your wound or around it:
- Increasing redness or swelling
- Increasing discomfort and pain
- Skin that is hot to the touch
- Yellow or green drainage
- Bleeding that doesn’t stop after applying pressure
- Foul odour
- If the lesion appears to have opened
- Rash
- Blistering
- Any questions or unexpected problems

Skin Graft
Wound Care after Graft surgery
After your skin graft surgery, you will have two surgical wounds to look after, the donor site and graft site. Each needs special care:
Graft Site
- Leave the dressing dry and intact until suture removal
- You may shower, but cover the dressing with plastic or a temporary waterproof dressing
- It is important the dressing does not get wet.
Donor Site This is the area that the skin was taken from.
- Leave the original dressing dry and in place for 3 days
- You may shower but cover the dressing with plastic or temporary waterproof dressing
- Make sure hands are washed thoroughly with soap & water before attending wound care
- After 3 days follow these steps:
1. Remove the dressing – soak dressing off in shower
2. Wash gently as normal or bathe with saline solution.
3. Allow to dry;
4. Apply a thin layer of Vaseline over sutures to keep moist;
5. If exposed to a dirty/dusty environment cover wound with a dry, non-stick dressing;
6. Repeat steps 1 to 5 every day until removal of the sutures.
Bleeding • If Bleeding occurs, apply firm pressure to the area for 30 minutes • Stay still • If persists, call the surgery
Pain relief Do take – Paracetamol or codeine based medication (as directed). Avoid aspirin and anti-inflammatory medications (unless prescribed by your Doctor)
Infection Please contact the surgery as soon as possible, if any signs of infection occur such as:
- Increasing redness
- Increasing Pain
- Hot to touch
- Oozing
Wound Repair
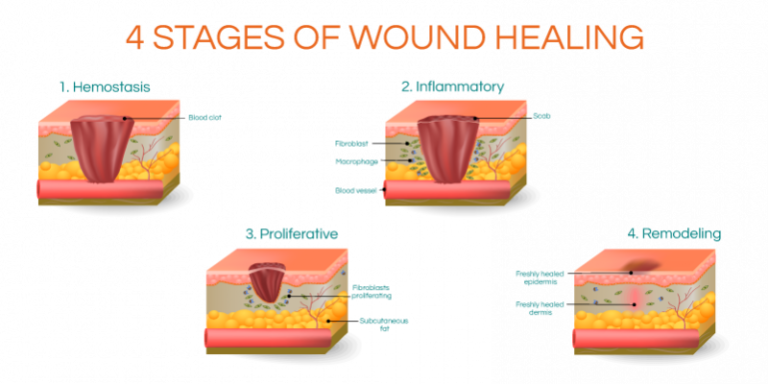
Wound healing is a physiological phenomenon that has a time course over six months. Scar continues to change for up to two year. The first phase of wound healing is called the inflammatory phase which occurs within the first 3 days of the wound healing; it is body’s normal response to injury causing heat, redness, swelling and oozing. Second phase of wound healing , within 3 – 24 days is when the wound is healing and body makes new blood vessels covering the surface of the wound. Wound is reconstructed and become smaller as it heals. Third phase is called maturation (24 days to 1 year), when building blocks are aligned and reorientated into optimal configuration to best resemble the normal tissues. Scar will mould, remodel and improve for a period of several years. The wound at this stage is still at risk and should be protected where possible.
Factors Affecting Wound Healing
There are several factors that can influence scar healing and appearance, including: Genetic : Some people intrinsically form better scars than others. This can depend on the skin type or may be independent of it. Abnormal healing responses are genetically controlled and include hypertrophic and keloid scarring. Patients can suffer from an inherited tendency to develop hypertrophic scars. These are scars that become red and raised and hard despite initial good healing. Certain areas of the body are more prone to this type of healing than others. Factors such as tension and infection may contribute to these hypertrophic scars. Hypertrophic scars will tend to flatten, soften and pale with time but this may take up to one to two years. keloid scar is another inherent disorder of healing. In a patient who forms keloid scars the wound will initially appear to heal without any problem. After a period of usually four to six weeks the scar will become red, raised, hard and may actually grow beyond the margins of the original wound. As if the scar has become a tumour. There is a defect in the healing mechanism where the scar is not turned off. Scar is continued to be produced even though the wound is healed. Another factor is the skin colour. The darker the skin the higher the risk. The body site of the scar is also very important for the formation of keloids; central chest area has the highest risk. Factors which have been shown to limit or control the formation of keloids and hypertrophic scars include pressure, (taping, massage, garments), silicone sheeting, intralesional steroids (injected into the actual scar) and radiotherapy of the scar after removal and resuture. Smoking and Nicotine Substitution Products : Nicotine narrows blood vessels and reduces blood flow to healing wounds. Smoking should be avoided in the perioperative period to optimise wound healing and may be critical in some operations to avoid death of tissues. Body Site: Extreme tension may be exerted on the skin as a part of normal daily activities. This tension placed on a healing wound will tend to stretch the wound out in the healing phase and result in a wide and depressed scar. Mobile areas with strong muscles are the most susceptible to the scar stretching and include the knee, shoulder and back. The scars in these areas that are susceptible to stretch and may heal with a fine line initially but over a period of weeks to months may stretch out. Surgeon: Surgeons are trained to optimise scars by thorough planning of the site and orientation of the scar, as well as using careful technique. Where possible designing an operation to place a scar in a hidden area is a great technique for making scars inapparent. Even most experienced plastic surgeons do not have magic wands and there may be patient’s genetic factors and site of the incision or wound which may overpower any technical expertise of the surgeon. Infection: Wound infection prevents wound healing and may produce an unfavourable scar. Nutrition: Patients who are deficient in vitamin E, vitamin C and protein will not heal normally. As long as an adequate level of all these nutritional factors are present the patient will heal well. Patient Motivation: Many of the abnormal healing responses such as hypertrophic and keloid scars develop after the wound initially appears to heal satisfactorily. The essential issue to any post-operative scar management is prevention. Measures should be introduced to prevent the scar getting bad, not introduced to try and fix it once it is bad. Thus if a scar is deteriorating, getting red or raised in the post-operative period the patient should inform the doctor so that appropriate measures can be employed.
How to improve the appearance of scars
Scars will improve with time. Sutures may be removed at one or two weeks but the process of wound healing continues on for up to two years. Lesions on the face will fade quickly, other areas will be slower. Several strategies can be undertaken to minimize the prominence of scars, including: Pressure: Applying pressure on a wound flattens it.. Pressure can be applied by massaging or taping the wound. Massaging is most effective when it is done often, for long periods of time, and with firmness. The wound can be massaged after sutures are removed and the tenderness is settling down. Taping may support the wound and prevent stretching but probably applies a small amount of pressure continuously. Taping with paper tape is usually adequate and very effective. Avoid UV: Sunlight damages skin and damages healing wounds. Healing wounds exposed to the sun will tend to glow red and may even get hyper pigment. After the wound has healed application of sunscreen SPF30+ is very important. This sun block may be contained in a cosmetic and used for camouflage of the healing wound. Lasers: Laser can be effective under the right circumstance to reduce the redness of scars and in certain circumstances to be used as a resurfacing tool to fade scars into the surrounding tissue. Again the particular type of scarring that has occurred will dictate whether a laser is an appropriate adjunct to optimise a scar or not.


