Melanoma
Melanoma is the least common type of skin cancers ( 1-2% of cases) but it is the most dangerous form of skin cancer and can spread rapidly.
Melanoma is characterised by uncontrolled growth of melanocytes. These are the cells in our skin that produce pigment which colour skin, hair and eyes. Melanoma is the most aggressive form of skin cancer.
The most common place for melanoma is on the skin of men’s backs or on women’s legs, however melanoma can occur anywhere on the body, including the head and neck, the skin under the fingernails, and even the soles of the feet or palms of the hands.
Melanoma is treatable if detected early but if the cancer spreads to other parts of the body (metastasises) the prognosis is poor.
Melanoma statistics
- Melanoma represents 2% of all skin cancers, but causes 75% of skin cancer deaths.
- Almost 20000Australians are expected to have been diagnosed with melanoma in Australia in 2022.
- Melanoma can spread rapidly and can be life threatening if left untreated.
- One person every six hours will die from melanoma in Australia.
- Melanoma is the most common cancer in Australian’s aged 15 – 44
- If diagnosed and treated early melanoma is nearly 100% curable
Early detection is important in order to start treatment before it metastasizes. Anyone of any skin colour can develop melanoma, though it is more common in fair-skinned people. A history of sunburns during a young age has been shown to increase the risk of developing this extreme form of skin cancer. Melanoma often has an irregular edge or surface, and it may be blotchy and brown, black, blue, red, white or light grey. Left untreated, a melanoma may spread deeper into the skin where cancer cells can escape and be carried in lymph vessels or blood vessels to other parts of the body.
A common sign of melanoma is a change to the size, shape, or colour of a mole, though not all melanomas develop in or near an existing mole. In some cases, a sudden, new growth on the skin can be melanoma.

Who is at risk of melanoma?
Australia has amongst the highest incidence of skin cancer in the world. 1 in 14 for males and 1 in 22 for females will develop melanoma,
- Fair skin that burns easily
- Light hair and light-coloured eyes
- Moles- Particularly if you have 50 to 100 or more and have any unusual or irregular looking moles that are typically larger in size
- History of sunburns or indoor tanning use
- Blood relatives who have had melanoma
- A weak immune system due to disease, organ transplant, or certain medications
- Previous history of melanoma or another skin cancer
- 50 years of age or older

Calculate your risk of melanoma
It’s important to get to know your skin. Examining your skin will help you notice changes and learn what is normal for you. Skin cancers that are found and treated early will need less invasive treatment and have a better outcome. Make it a habit to examine over your skin every 3 months.
Melanoma institute Australia has developed a online risk assessment tool to calculate your risk of melanoma. Click on the following icon or this link here to assess your own risk.
Signs of melanoma
- A lesion that just doesn’t look like any other spot on your body – a so called “ugly duckling”
- A mole that is changing (in size, shape, colour or texture)
- A spot that is tender or recurrently bleeds, get crusty or heals then breaks down again
- A skin lesion that is elevated, firm and growing
Different forms of melanomas
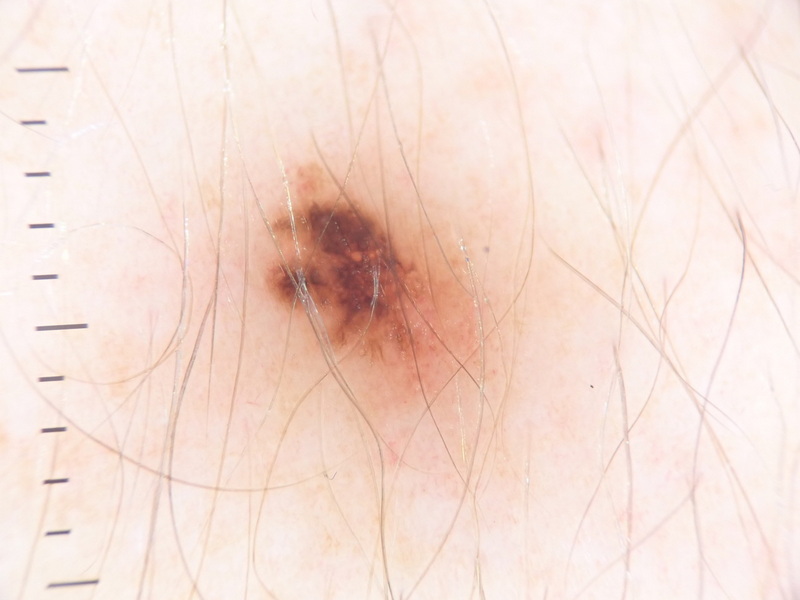
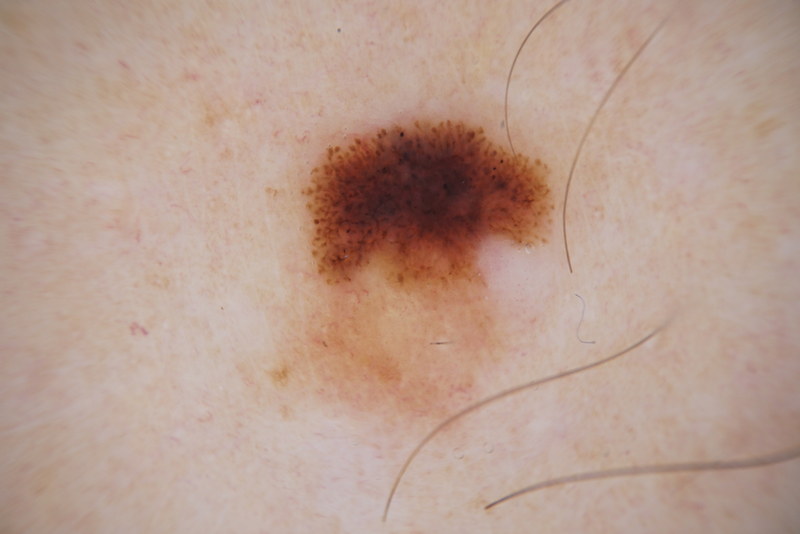
- Superficial spreading melanoma: This is the most common form of melanoma representing roughly 70% of all cases. This type of melanoma undergoes a long radial growth phase prior to invading deeper into the skin, reaching the dermis, and posing a threat of distant spread via the blood stream or lymphatic system. They can develop a vertical growth phase over time. Superficial spreading melanomas are typically characterised by a lesion with irregular borders and uneven pigmentation.
- Nodular melanoma: This is the most aggressive form of melanoma as it undergoes no radial growth phase and instead enters a vertical growth phase from the outset. Nodular melanomas have a raised, nodular lesion with irregular patches of colour and an irregular border. About 20% of nodular melanomas may not have any pigment and this can make diagnosis more difficult.
- Lentigo maligna melanoma: The least aggressive melanoma due to its long radial growth phase. Lentigo maligna melanoma is commonly found on older people who have worked in an outdoor occupation. These occur on areas of the body that have received a lot of sun exposure and are therefore most common on the face, ears, neck and head.
- Acral lentiginous melanoma: This type of melanoma is found on the soles of the feet, on the palms or under the fingernails. It is the most common form of melanoma in Asians and black skinned people. it is more aggressive than superficial spreading melanoma and less aggressive than nodular melanoma.





Melanoma in Australia
Melanoma of the skin incidence rates have increased from 54 cases per 100,000 people in 2000 to an estimated 69 cases per 100,000 people in 2023. In 2023, it is estimated that 35% of melanoma of the skin cancer cases are diagnosed on the trunk of the body, 26% on the upper limbs (including shoulder), 18% on the lower limbs (including hip) and 7.6% on the scalp and neck.
The proportion of melanoma of the skin diagnosed by site varies by sex. For example, in 2023 it is estimated that 25% of melanoma of the skin cases are diagnosed on the lower limbs (including hip) for females while for males it is 13%. Conversely, the trunk accounts for 41% of the cases for males and 27% for females.
Melanoma of the skin incidence rates for females are estimated to be 56 cases per 100,000 females in 2023 while male rates are 85 cases per 100,000 males.
Melanoma of the skin incidence rates have been decreasing for people under 40 since the late-1990s. Incidence rates for people aged 40 to 49 ranged between 44 and 53 cases per 100,000 people since the mid-1990s. Rates for people aged 50 and over continue to rise.
The ‘Slip Slop Slap’ campaign was a very large skin cancer awareness and prevention campaign commencing from the early 1980s. In 2023, the population aged under 40 were born after or around the ‘Slip Slop Slap’ campaign and have spent their lives in an environment where skin cancer awareness has been greater. Skin cancer awareness and prevention advice continues today. While populations over 40 have increasing incidence rates, the rate increases are greater for the oldest populations who are likely to have spent more of their lives in times when there was less skin cancer awareness.
After many years of increasing, melanoma of the skin mortality age-adjusted rates peaked at 8 deaths per 100,000 people in 2013. In 2023, the estimated age-adjusted mortality rate is 5 deaths per 100,000 people. The reduction in mortality rates is accompanied by reductions in the number of deaths (1,625 deaths in 2013 and an estimated 1,300 in 2023).
Since 1995–1999, 5-year melanoma of the skin survival rates have been a little over 90%. The melanoma of the skin 5-year survival rate for 2015–2019 was 94% and is the highest rate recorded for melanoma of the skin.
Melanoma myths
“When a melanoma is cut out, it’s gone”
It’s important to get melanomas surgically removed early, but preventing a melanoma from occurring in the first place is even more important. After surgical removal of melanoma, regular skin checks are very important. Your doctor will give you an individualised plan on further check ups. Melanoma cells can burrow into the blood stream or lymphatic system and spread. Once they’re circulating around your body they can reappear months or years later – often in the lungs, liver and brain.
Sunscreen is all I need
The use of sunscreen is just one of the five skin protection measures you should use every day. Look on it as an extra form of protection, not your primary sun protection measure and certainly not your only one. Stay in the shade and avoid the sun during peak UV times. Wear protective clothing, a broad brimmed hat and sunglasses. Use a SPF30+ broad spectrum, water resistant sunscreen on all areas of exposed skin. Reapply sunscreen at least every 2 hours, and after swimming. Use water resistant sunscreen if you participate in water sports or sweat often.
Solariums
Using a solarium, sunbed or tanning bed to tan is not any safer than sun tanning. Solarium can increase your risk of a melanoma because sunbeds also emit UVA and UVB radiation from above and below your body.
I’m healthier with a tan”
You may think you feel or look healthier with a tan but once you understand what is happening to your skin, you’ll think again. Tanning is skin cells in trauma. In response to UV damage, skin cells produce melanin to protect themselves. However, one damaged cell can start a deadly melanoma growing. Too much UV exposure can result in structural damage to your skin – in the short term, burning or scarring and in the long term premature ageing or skin cancer. There’s nothing healthy about a tan.
I need lots of sun to get Vitamin D
We all need Vitamin D for good health and the main source for Australians is the sun. However, the vast majority of us will get all the Vitamin D we need, not by tanning but just going about our normal daily activities while still protecting our skin in the five ways below.